Traditionally done on paper, surveys are a common way to collect data from study participants. Surveys are questionnaires that allow data to be collected from a pre-defined sample in a population [1].
Patient reported outcome measures, or PROMs, are a form of clinical outcome assessments (COAs) an easy method for measuring a patient’s health status or health-related quality of life. These capture data from moments in time through questionnaires which patients complete independently [2].
In the past, surveys have been administered on paper, which requires tedious administration and several logistics, and also poses a private health information security risk. However, due to digital technology, collecting ePROs (electronic Patient Reported Outcomes) securely is easier than ever. Patients can complete secure surveys sent via email, saving time, increasing engagement, and requiring less administration. At the moment, 23% of studies in Castor are using surveys through our eCOA / ePRO platform.

Benefits and Challenges of eCOA / ePRO
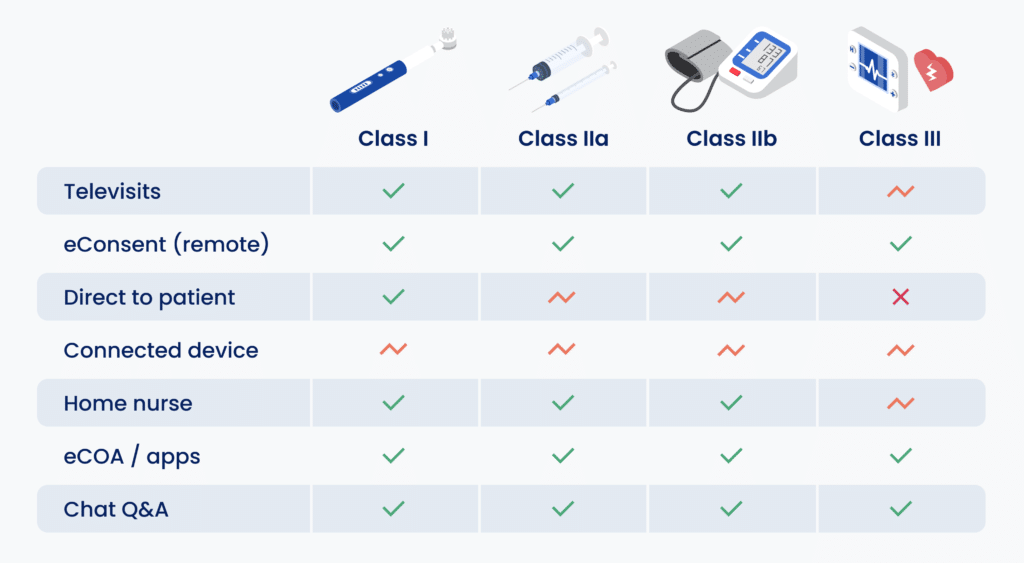
Online surveys are easy to distribute, however researchers should use tools designed and built for medical research, both for security and data compliance. A major benefit is a more efficient and streamlined workflow, equating to time saved for researchers and participants. Often, for example, travel time to clinic for data collection can be a barrier for participants and negatively impact the study, especially when researching rare diseases or small gene pools [3].
Surveys are cost effective, requiring minimal research power to reach people and collect data. With the correct electronic data capture (EDC) tool, researchers can send surveys directly from the system and do not need to import or copy data from paper. Well designed surveys will collect high quality relevant research data, but require careful crafting and evaluation of wording and questions [4].
As discussed above, questionnaires need to be well crafted to ensure they are valid and reliable. It is also important to ensure that the correct population sample is selected. As with all study designs, surveys can introduce bias as a result of poor responses or no-responses (response bias).
How to create good surveys

As researchers, the challenging task lies in creating a well designed questionnaire that measures what it claims to measure ensuring that it is valid. External validity is important for the generalizability of the study, ie. are the inclusion or exclusion criteria properly defined, can the results be applied to a population [4]. And internal validity is related to the robustness of the study, ie. does it have sufficient statistical power, proper control groups, randomization and blinding [4]. And a reliable questionnaire that will produce consistent results upon repetition [1].
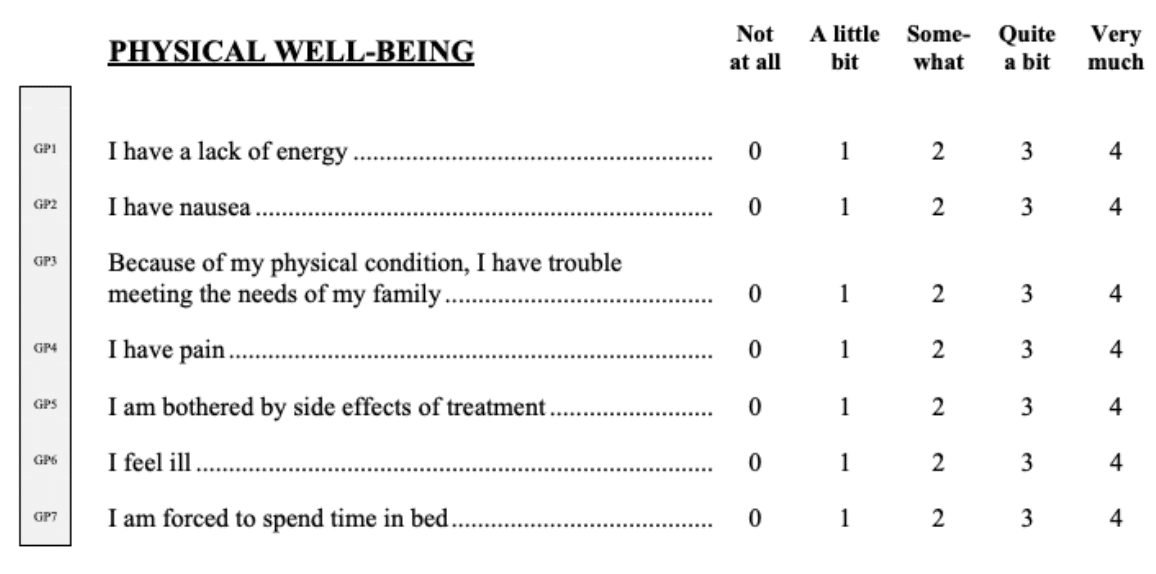
When generating a questionnaire, the questions can be close-ended or open-ended. With close-ended questions, researchers set the range of answers on a scale or a range of tick-boxes [1]. Open-ended questions or free text can enrich quantitative data, and researchers will want to plan in advance how this data will be analyzed [1].
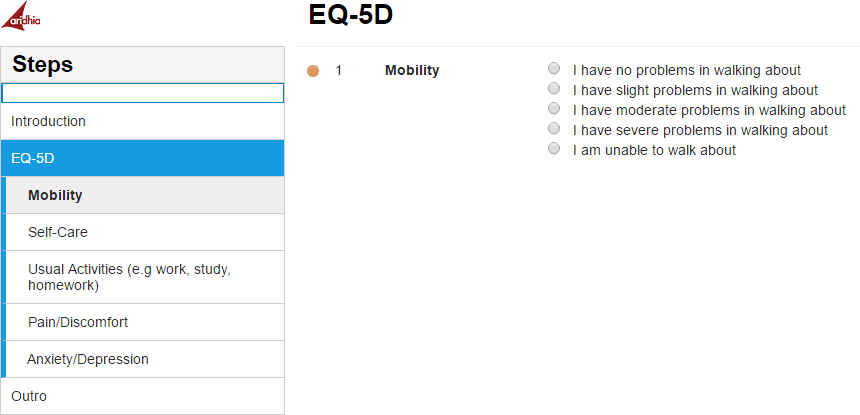
Standardized questionnaires can also be used, see an example below of an EQ-5D Questionnaire from Kieran Bond of Aridhia [2]. These widely used forms ensure that a high level of validity and reliability is achieved throughout the research.
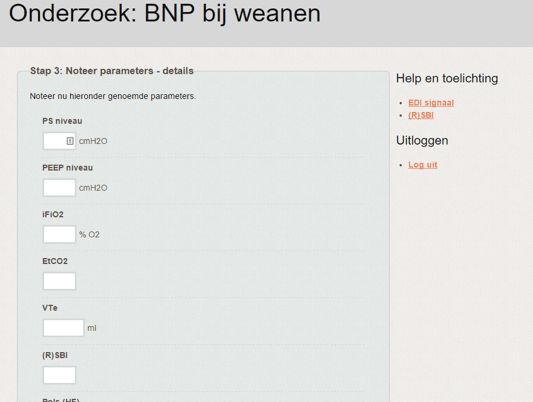
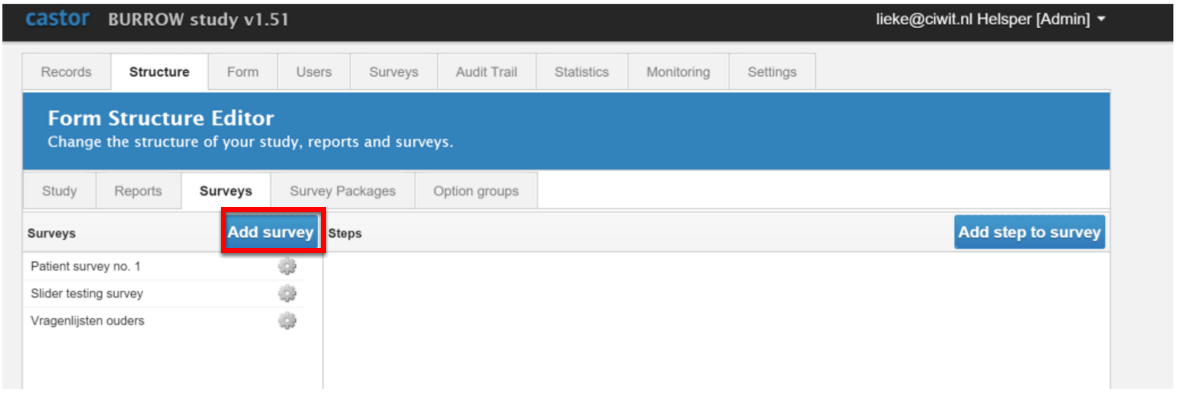
Using surveys for research in Castor eCOA / ePRO
Users can choose from tried and tested questionnaires shared by Castor users in the Castor Form Exchange. Standardized forms, such as the 36-Item Short Form Health Survey (SF-36) that measures quality of life, can be easily downloaded and re-used. Researchers can schedule surveys and create emailing schedules to distribute patient questionnaires on certain dates or according to a custom timeline. Data from the surveys can be in a variety of formats (SPSS, Excel, CSV).
Using encrypted email addresses, clinical data entry is combined with outbound survey invitations sent to study participants. And at the push of a button, researchers can send a questionnaire to hundreds of participants, monitor its status and see results directly in the study dashboard.
Click here to find out more about the Castor ePRO features or check out our webinar on how to build surveys in Castor.
Sources:
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC420179/
- http://www.aridhia.com/blog/building-trust-and-improving-participation-in-clinical-trials-using-innovative-electronic-data-capture-platforms/
- http://www.bmj.com/content/350/bmj.g7818
- http://www.bmj.com/about-bmj/resources-authors/bmj-right-journal-my-research-article